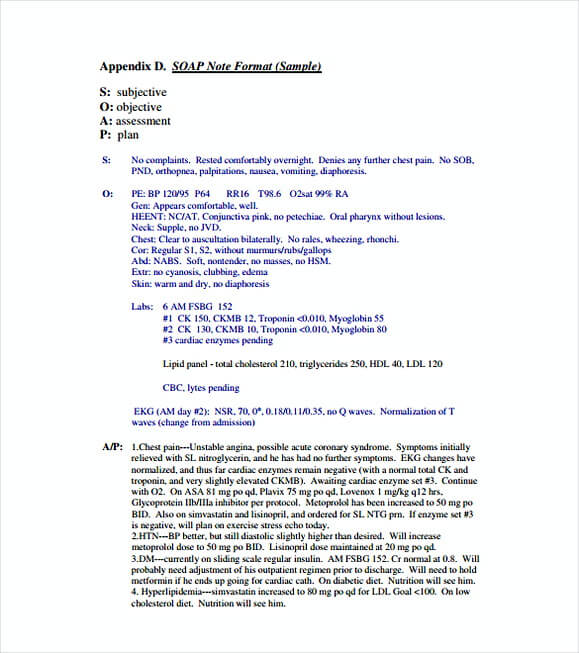
What is A SOAP Note?
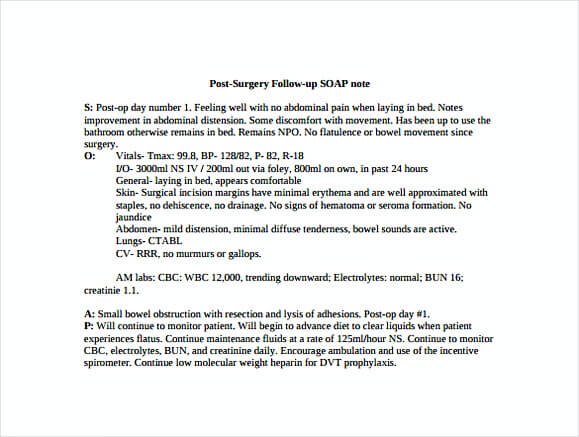
A SOAP note is an acronym of Subjective, Objective, Assessment and Plan which represents a method of documenting a patient’s health record by the healthcare provider. This is an organized and structured way to file the patients’ data done by the doctors and nurses.
The origin of this method was introduced by Larry Weed around 50 years ago which he reminds the clinicians to do specific tasks while giving the outlook of information to be evaluated. Besides, this is very useful for other healthcare to diagnose, assess and give treatments to the patients later. In short, you can understand the SOAP definition bellow before using our soap note template.
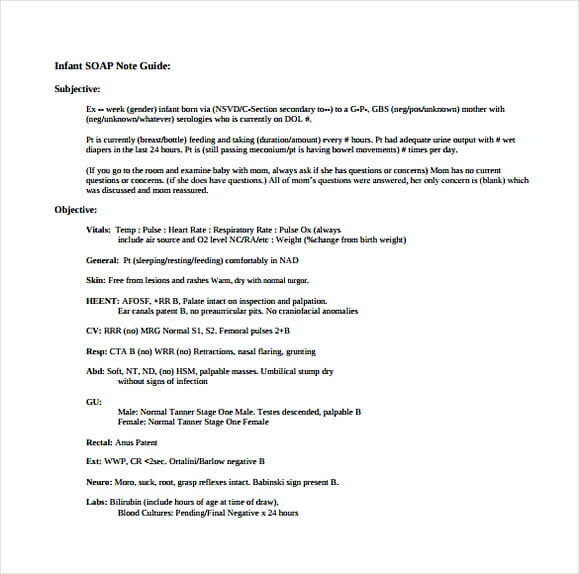
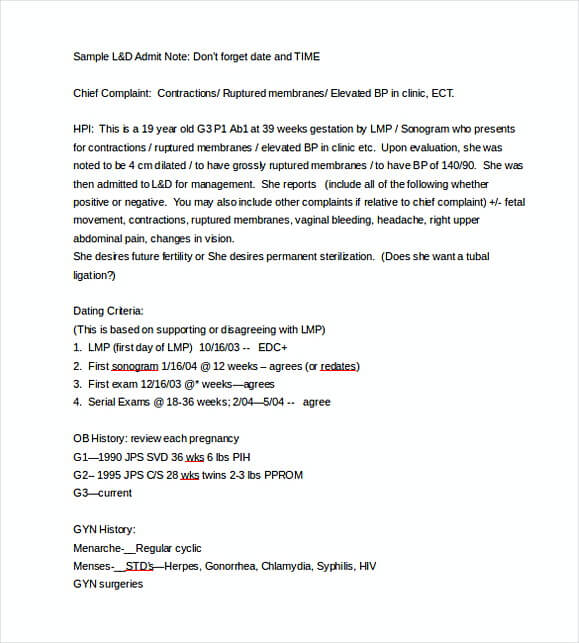
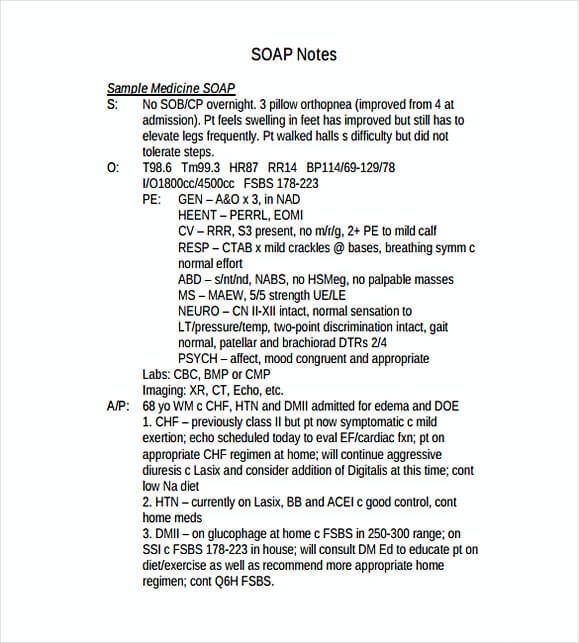
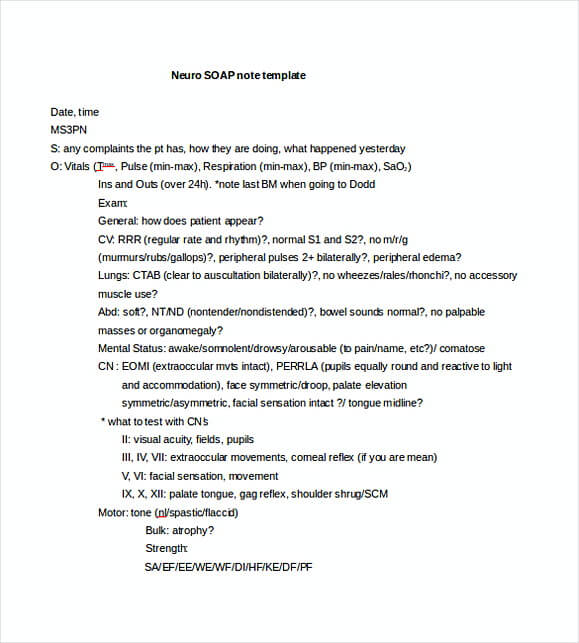
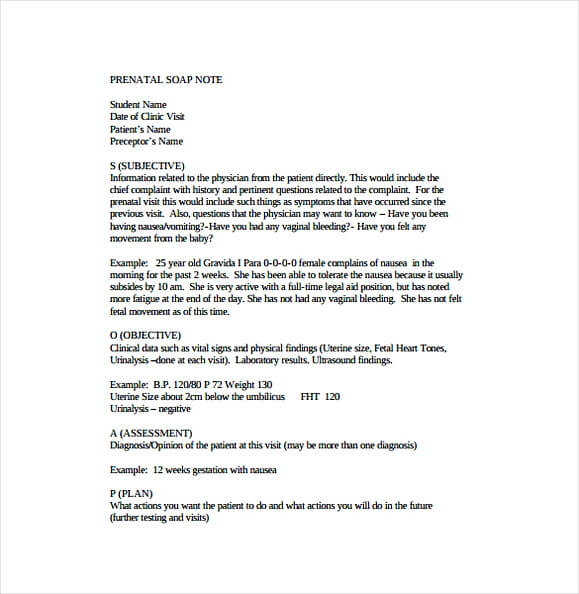
- Subjective – The word subjective means what patients should say with the problems, procedures, intervention, concern, and issue.
- Objective – The objective refers to what the healthcare have observed including the ongoing treatments or intervention that have been done.
- Assessment – This means the analysis related to the different components of the assessment.
- Plan – The plan relates to the procedures that will be used for a successful treatment.
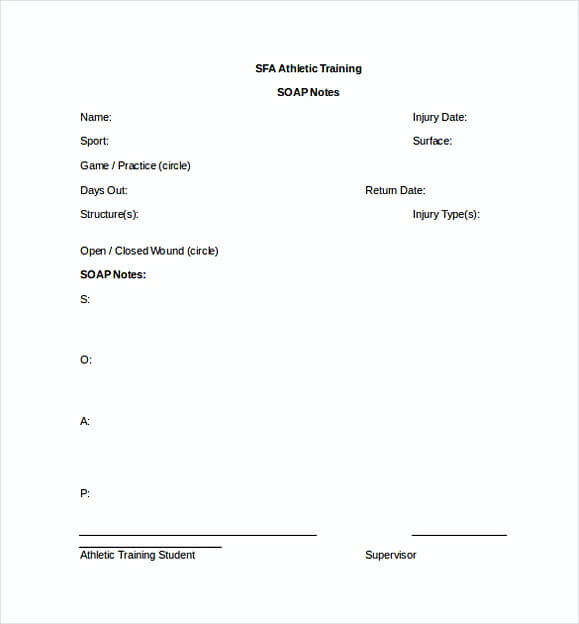
Using the soap note template is not only limited to the nurses and doctors, but other health professionals can also use it as well including the physicians, counselors, nurse practitioners and so on. By using this procedure, every healthcare can ensure that the procedure is more accurate.
What Are The Benefits of Using SOAP Note Template?
Generally, as we said in the early of this article, the SOAP note template helps you keep on track and evaluate what has been done to patients. In this case, you will know the progress and also other things that beneficial to the patient’s improvement:
- Giving Important Details – Having this document will let you and other healthcare know whether the patients are taking the regular treatments or not. This can be legal proof in the patient’s health report which one day will be useful.
- Serving As The Evidence of Your Skills – Writing notes on the SOAP note template will let other physicians know that you have been successful in implementing procedures of treatments. Besides, when it is on the patients’ side, you have the proof when your patients’ family ask a question in the future.
- Serving As The Flexible Note – Writing the progress, condition and other interventions in your treatment procedures will give the overall overview and improve the method what can be done to help your patients.
In writing a SOAP note, there some components to be included, which are subjective, objective, assessment, and plan as you see on the above definition. It is quite easy and very systematic for your work so other healthcare can read and understand quickly when you are not in charge which this might help the patients to get cured sooner. Additionally, a mindful decision can be made using this method.
If you want to download our template, just hit the thumbnails of the download buttons. You don’t need to register.